Prostate Cancer: Symptoms, Causes, Risk Factors, Diagnosis, and Treatment
Category : Prostate Cancer | Sub Category : Prostate Cancer Posted on 2025-07-02 11:16:21
Early-stage prostate cancer is often asymptomatic. As the disease progresses, the following symptoms may emerge, warranting consultation with a healthcare provider:
Frequent or urgent need to urinate, particularly at night
Weak or interrupted urine flow
Pain or burning during urination (dysuria)
Urinary incontinence
Fecal incontinence
Painful ejaculation or erectile dysfunction
Blood in urine or semen
Pain in the lower back, hips, or chest
Causes
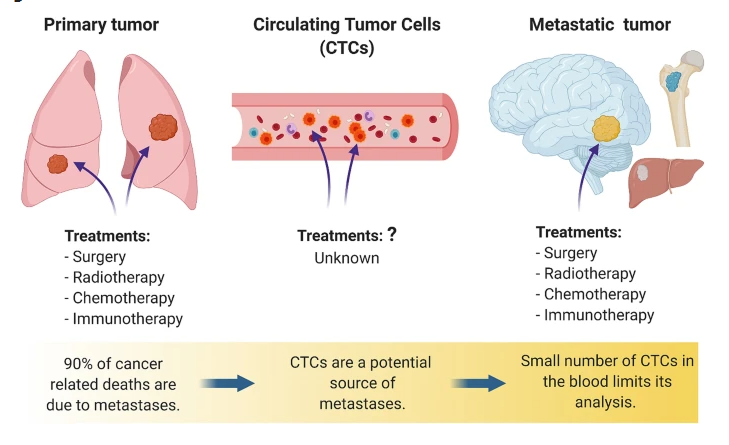
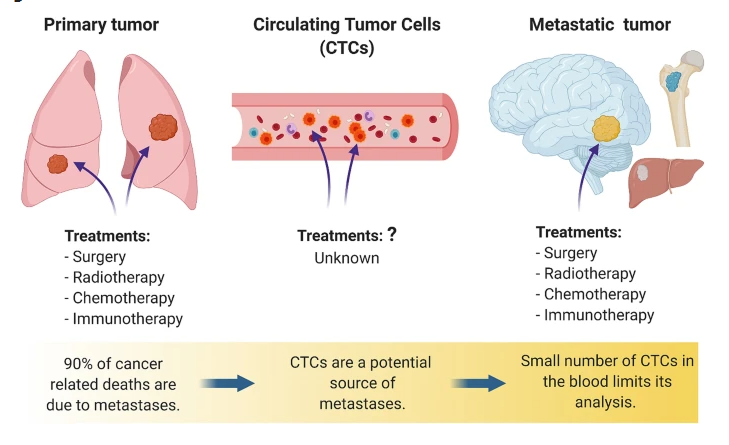
The precise cause of prostate cancer remains unclear. It develops when prostate cells divide abnormally and at an accelerated rate. Unlike normal cells, cancer cells do not die but multiply, forming a tumor. These tumors may metastasize, spreading to other parts of the body. Most prostate cancers grow slowly and are often diagnosed before spreading beyond the prostate, making them highly treatable at this stage.
Risk Factors
Key risk factors for prostate cancer include:
Age: Risk increases with age, particularly after 50, with approximately 60% of cases diagnosed in individuals over 65.
Race and Ethnicity: Black individuals or those of African descent face a higher risk, particularly for aggressive cancers diagnosed before age 50.
Family History: A two- to three-fold increased risk exists if a close family member has had prostate cancer.
Genetics: Conditions such as Lynch syndrome or inherited mutations in BRCA1 and BRCA2 genes elevate risk.
Other potential risk factors with less conclusive evidence include:
Smoking
Prostatitis
Obesity (BMI > 30)
Sexually transmitted infections
Exposure to Agent Orange
Diagnosis and Testing
Prostate cancer is diagnosed through screening tests, physical examinations, imaging, and, if necessary, a biopsy. Screening typically begins at age 55, or earlier for high-risk individuals, and generally ceases after age 70. Diagnostic methods include:
Digital Rectal Exam (DRE): A provider palpates the prostate for abnormalities.
Prostate-Specific Antigen (PSA) Test: Elevated PSA levels may indicate cancer, though benign conditions like benign prostatic hyperplasia or prostatitis can also raise levels.
Imaging: MRI or transrectal ultrasound visualizes suspicious areas in the prostate.
Biopsy: A tissue sample is analyzed to confirm cancer and assess its aggressiveness. Genetic testing of the sample may guide treatment.
Grading and Staging
Gleason Score: Evaluates the abnormality of cancer cells, indicating the cancer’s potential aggressiveness.
Cancer Staging: Determines the extent of cancer spread, classified as local (confined to the prostate), regional (invading nearby structures), or metastatic (spread to bones, lymph nodes, liver, lungs, or other organs).
Management and Treatment
Treatment is tailored based on the cancer’s stage, growth rate, and the patient’s overall health. A multidisciplinary team, including urologists, radiation oncologists, and medical oncologists, may be involved. Early-stage cancers are often curable.
Surveillance
Active Surveillance: Involves regular screenings, scans, and biopsies every 1–3 years for low-risk, early-stage cancers without symptoms.
Watchful Waiting: Used for older patients or those with comorbidities, focusing on symptom management with less frequent testing.
Surgical Interventions
Radical Prostatectomy: Removes the prostate gland, either via open surgery (single abdominal incision) or robotic-assisted surgery (multiple small incisions). Effective for non-metastatic cancers.
Radiation Therapy
Brachytherapy: Radioactive seeds are implanted in the prostate to target cancer cells.
External Beam Radiation Therapy (EBRT): Delivers targeted X-rays to the tumor, with advanced techniques like IMRT minimizing damage to healthy tissue.
Systemic Therapies
Hormone Therapy: Reduces testosterone levels through medication or orchiectomy to slow cancer growth.
Chemotherapy: Uses drugs to kill cancer cells, often for advanced or metastatic cases.
Immunotherapy: Enhances the immune system’s ability to target cancer, typically for advanced or recurrent cases.
Targeted Therapy: Focuses on genetic mutations (e.g., BRCA) to inhibit cancer growth.
Focal Therapies
Emerging treatments for low-risk, localized tumors include:
High-Intensity Focused Ultrasound (HIFU): Uses sound waves to heat and destroy cancer cells.
Cryotherapy: Freezes cancer cells within the prostate.
Laser Ablation: Applies intense heat to eliminate tumors.
Photodynamic Therapy: Uses light-sensitive drugs and specific light wavelengths to kill cancer cells.
Side Effects of Treatment
Common side effects include:
Incontinence: Urinary leakage or urgency, typically improving within 6–12 months.
Erectile Dysfunction: Treatment-related impacts on erections, often manageable with medications like sildenafil or tadalafil.
Infertility: Potential impact on sperm production or ejaculation, with sperm banking recommended for those planning future parenthood.
Patients should discuss side effects with their healthcare team, as interventions are available to mitigate these issues.
Disclaimer
This information is provided for general informational purposes only and does not constitute professional medical advice. It is not a substitute for consultation with a qualified healthcare provider. For medical emergencies, contact your physician or, in the United States, call 911 immediately.
Leave a Comment:
SEARCH
Categories
Recent News
- Cancer Pain Medications
- Gastric Cancer (Stomach Cancer)
- New Discovery Links Mitochondrial DNA to Immunotherapy Success in Cancer Treatment
- John’s Journey: Healing Through Lifestyle and Natural Remedies
- The truth about finding a cure for cancer
- Federal Government Commissions Three Oncology Centres to Strengthen Cancer Care in Nigeria
- Nigeria Advances National Cancer Control Efforts
- Nigeria’s Biggest Cancer Awareness Walk by Mukhtasar M. Alkali
READ MORE
2 months ago Category : Tell us your Story
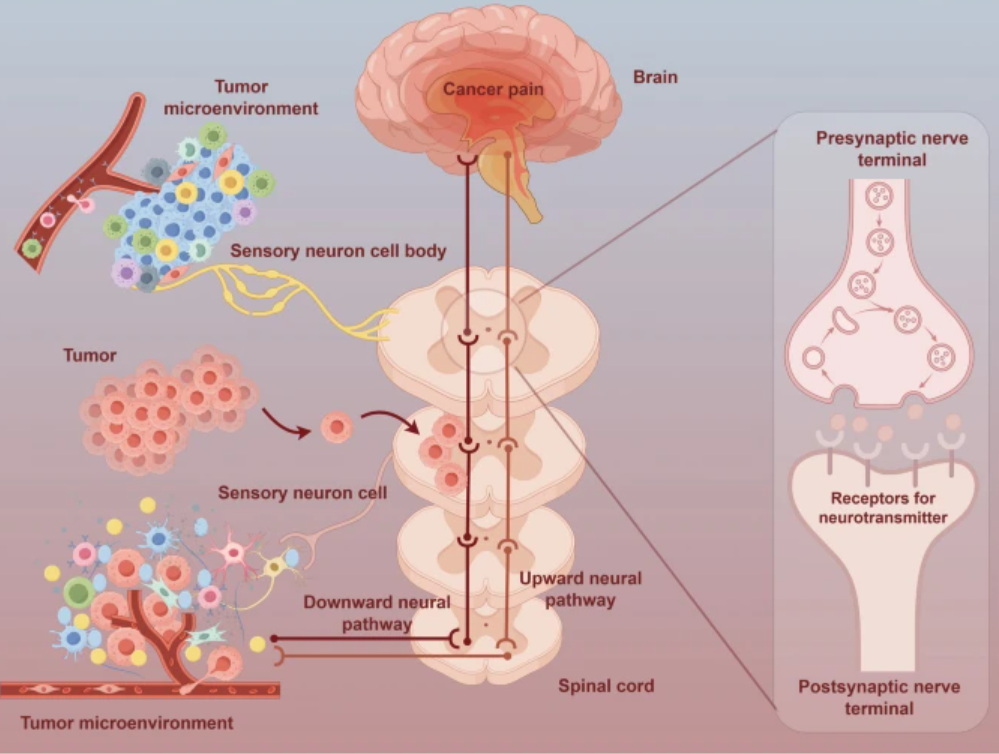
Cancer Pain Medications
Read More →2 months ago Category : Gastric Cancer

Gastric Cancer (Stomach Cancer)
Read More →3 months ago Category : Colorectal Cancer
New Discovery Links Mitochondrial DNA to Immunotherapy Success in Cancer Treatment
Read More →3 months ago Category : Tell us your Story